 Lots of ocular problems are related to retina disorders. Macular degeneration and diabetic retinopathy are only some of the many retina complications. Retina Specialist Dr. Lauren Kallina of the New Jersey Eye Center has kindly agreed to fill us in on some of the problems afflicting today’s patients.
Lots of ocular problems are related to retina disorders. Macular degeneration and diabetic retinopathy are only some of the many retina complications. Retina Specialist Dr. Lauren Kallina of the New Jersey Eye Center has kindly agreed to fill us in on some of the problems afflicting today’s patients.
The following is a transcript of the interview.
Can you tell us a little about your job and what your job actually entails?
I’m an ophthalmologist. My sub-specialty is retina. Most of our patients are diabetic, suffering from diabetic and macular edema or macular degeneration of the dry or wet type. A good percentage are 55 and over, although we have quite a few 48-60-year-olds with uncontrolled diabetic retinopathy. Many patients come in, not knowing the extent or the risk of the diabetic retinopathy that they can have. Often they come in with a lot of diabetes not previously diagnosed elsewhere.
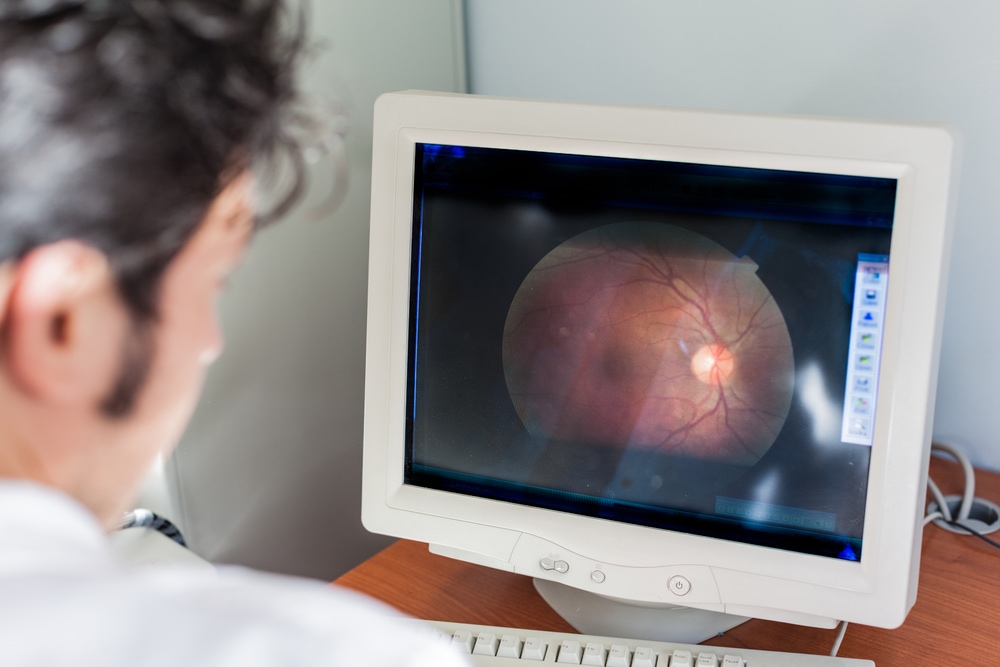
A diabetic baseline examination would involve of course, looking at the eye, examining the eye with indirect ophthalmoscopy. Then they move on to ocular appearance testing, which looks into the thickness of the macula. A diabetic can have diabetic macular edema, which requires specific treatment. Then we move on to fluorescein angiography. This involves checking the retinal circulation by forcing fluorescein dye into the eye, injected via the hand or arm vein running to the eye. We can treat that here, as well as severe perfusion prolific diabetic retinopathy. We are able to treat diabetic macular edema with intraocular injections. A lot of diabetic patients also require laser procedures.
Another common diagnosis is macular degeneration. Patients can have a dry form which only requires OCT [optical coherence tomography] testing, ocular tomography, and occasionally an angiogram. Patients with dry macular degeneration typically need only observation, maybe every six months, and repeat evaluation only or certain vitamins to stabilise them.
We can diagnose patients with wet macular degeneration right here on the spot with ocular tomography and fluoroscein angiography. Like patients with diabetes, they get treated with intravitreol or intraocular injections.
Another very common diagnosis I see is vein occlusion which may be related to hypertension or uncontrolled blood pressure. Vein occlusion can be mild or severe. Where it is severe, patients have a sudden loss of vision. Again they have retinal edema and that too requires similar treatment with intraocular injections. Many vein occlusion patients also require laser treatment or fluorescein angiography testing to look at their peripheral perfusion.
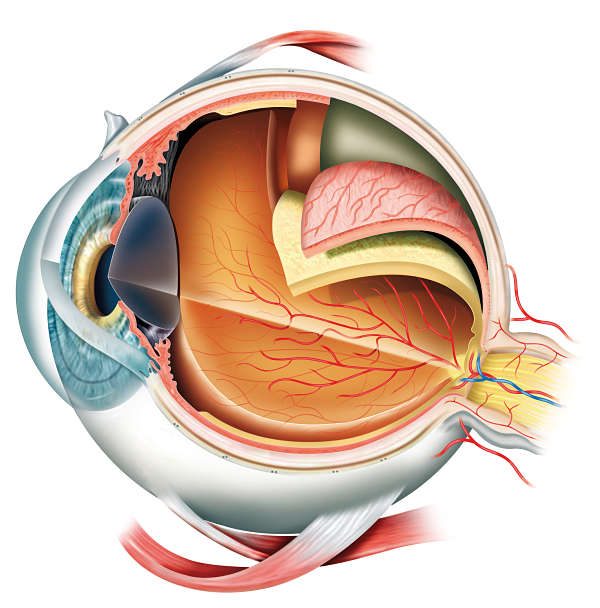
Posterior vitreous detachment is also one of the most common conditions, where a patient experiences sudden floaters and flashes of light, and this is a natural phenomenon. If the vitreous jelly in our eye starts to disintegrate, patients have flashing lights or floaters. With indirect ophthalmoscopy we can detect whether there is a more serious issue underlying this, such as a retinal tear, a retinal hole or vitreous haemorrhage. Significant symptoms would be loss of vision due to the floater or the haemorrhage. A vitrectomy operation can be performed to remove any consequential bleeding, but we only do vitrectomies for patients with posterior retinal detachment. If the patient is still troubled by these symptomatic floaters several months down the line, I do not opt to do a vitrectomy for floaters.
Another common diagnosis that we see in people who are very, very near-sighted, which is a high myope – typically near-sightedness of minus 5 or more, is typically lattice degeneration. This is a thinning of the retina on the periphery. This practice here also does laser vision operations. We have a high population of high myopes, because these are the patients who underwent laser surgery in the past.
Those are the top diagnoses that we see. We see many diabetics who are stable, who do not need treatment, and they come regularly about every six months. Patients with dry macular degeneration do not need treatment either. Generally they come for a check-up about every six months.
Are diabetic retinopathy and macular degeneration caused by a high insulin or sugar levels in the blood?
No, not a high insulin level. Even when a patient has had diabetes for more than 10 years, we still can see these abnormalities at the macrovascular level of the retina. There’s a whole very fine cascade of pathophysiologies that occur at a macrovascular level, including loss of pericytes around the retinal capilliary anti-vascular endothelial growth factor.
We use an anti-viral drug. The issue at hand is that inside the eye, when we inject vascular endotherial growth factor, we get an effect because we are blocking the abnormal hormone in the eye. All three of these entities have similar underlying pathophysiologies because of ischemia, generally because of the loss of normal blood flow.
If patients come urgently with flashes, floaters, not only do they have posterior retinal detachment, but they might have a retinal tear. We can of course do a laser procedure on the spot for a retinal tear or hole.
Can you tell us more about dry or wet macular degeneration?
We’re only just starting to understand the genetics of dry macular degeneration. It seems as though, at the retina’s most base level, the retinal pigment epithelium, there is a genetic abnormality whereby the by-products cannot be appropriately put back into the system. These waste products of that highly metabolic layer, called the retinal pigment epithelium, form drusen down at that layer.
Drusen are simply a cholesterol-like clump that gets deposited biochemically, because the underlying genetic defects are dry and they can remain stable. These can be small or large, in the centre of the eye or on the periphery. These drusen can lay dormant forever. If there is some reactivation of the drusen at the same level as the retinal pigment epithelium, abnormal vessels start to grow to help the circulation in the area. But the abnormal blood vessels simply grow and bleed without doing any good.
The ensuing wet form of macular degeneration is treated with Avastin, an anti-vascular growth medication originally used in oncology for stomach cancer. Some 15 plus years ago, it was found that some cancer patients were showing regression of other issues after chemotherapy. So, they continued taking this cancer drug in small doses experimentally. Since it was seen to regress the blood cells in tumors, it was injected into the eye similarly to prevent the development of abnormal blood vessels. This treatment was shown to be effective and safe.
Finally we do use intravitriol or intraocular steroids, should there be no improvement at all regarding issues like diabetic macular edema and secondary macular edema from vein occlusion.
What would you suggest that people who are worried about their eye conditions related to diabetes or macular degeneration should do?
If any patients have perhaps a history of macular degeneration in the family or any level of diabetes, it is urgent for them to have a baseline evaluation. Much of the underlying pathology is not evident simply from the state of your vision.
Many of retina problems, if detected early, can be reversed.
In many patients, when wet macular degeneration has been discovered early, it has resulted in a cure. I have many patients with early diabetic retinopathy that we are able to control, so there is no progression to the advanced stages.
You can read more about Diabetic Retinopathy Causes
Although ocular evaluation is most important, patients shouldn’t be shy about asking the general ophthalmologist for a retina exam because we do some more profound evaluations, looking for underlying pathology that might not be detected in a general optomotrist’s only office. But again, only if the symptoms are flashing, floaters, distortion or a family history of any of those such as macular degeneration and of course anyone who has diabetes. Many have had diabetes for two years plus, but it has gone undetected.
After a baseline evaluation, I would advise what procedure needs to be done. We are able to accommodate those patients for glaucoma filtering surgery. These are not normal glaucoma patients. They are very serious glaucoma patients with neovascular glaucoma resulting from diabetes who need intravitreal glaucoma filtering surgery with the implementation of a Baerveldt valve. Neovascular glaucoma needs to be treated early from the standpoint of flashes or floaters, when straight lines are curved, metamorphopsia, sudden loss of vision and severe pain in the eyes occur, or vision is clouded off to the side or a curtain falls down over the eye.